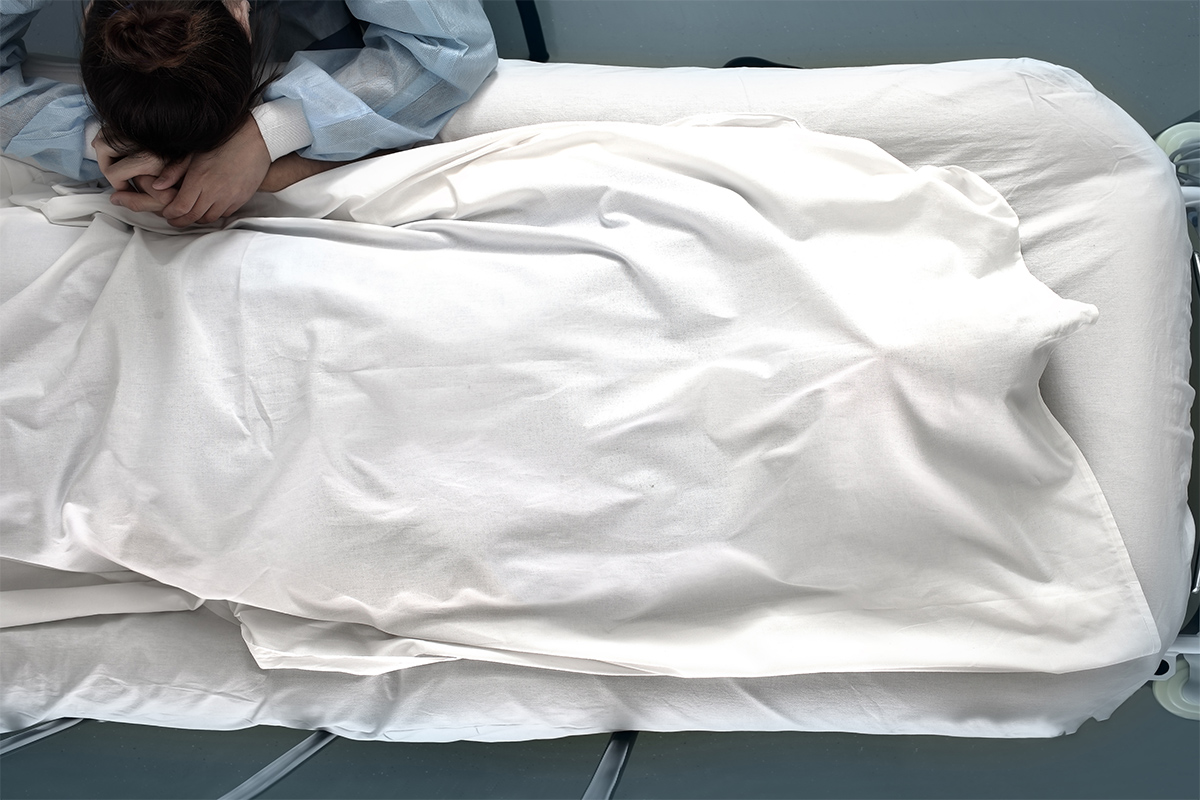
A medical team considers withdrawal of artificial nutrition and hydration supporting a 6-month-old girl with complex cardiac disease, devastating neurological injury, and ongoing, unmanageable pain. Diffuse neurological injury and severe ischemia in all four limbs offers a bleak prognosis. Drawing on the bioethics literature on the subject, the following case presentation and analysis illustrates how a medical team and family can approach such a situation.