
Overview of volume 32 issue number 1: Informed consent in neonatal clinical trials, home medical care, biases is data-driven medicine, patient worldviews, moral courage, and physician shadowing.

Use of sedation and restraints is sometimes the only means available to stabilize medically fragile eating disorders patients. While minors are not given the option to refuse care that competent adults are, forced tube feeding nonetheless challenges the minor patient’s senses of identity and control. The following case study chronicles the management of an 11-year-old patient transferred from inpatient child psychiatry unit to the adolescent medicine service for nutritional rehabilitation.

Conflicts between parents and health care providers are among the most common of the ethical issues encountered in pediatrics. In this article, three cases are presented along with an ethical framework for thinking about cases in which parents and providers disagree.

This paper presents guidance developed by a multidisciplinary group of bioethicists and patient advocates considering patient- and parent-centric approaches to informed consent in neonatal research in the context of an ongoing clinical trial for neonates with spinal muscular atrophy (SMA).

A lack of empathy while standing in as a translator for another physician’s patient and family raised the following question: can one be culturally insensitive to one’s own culture? The following narrative explores the divide between medical and patient/family worldviews.

A nurse recounts her experience as a new NICU nurse raising an issue about the appropriateness of a procedure with the rest of the medical team. The narrative addresses issues of power imbalance, ethical controversy, medical decision-making, and moral distress.

Overview of Pediatric Ethicscope 2018 Volume 31 Number 1: Embracing diagnostic uncertainty; ECMO referral; moral language following pediatric death; ethical issues in genetics research; Children’s Mercy Bioethics.

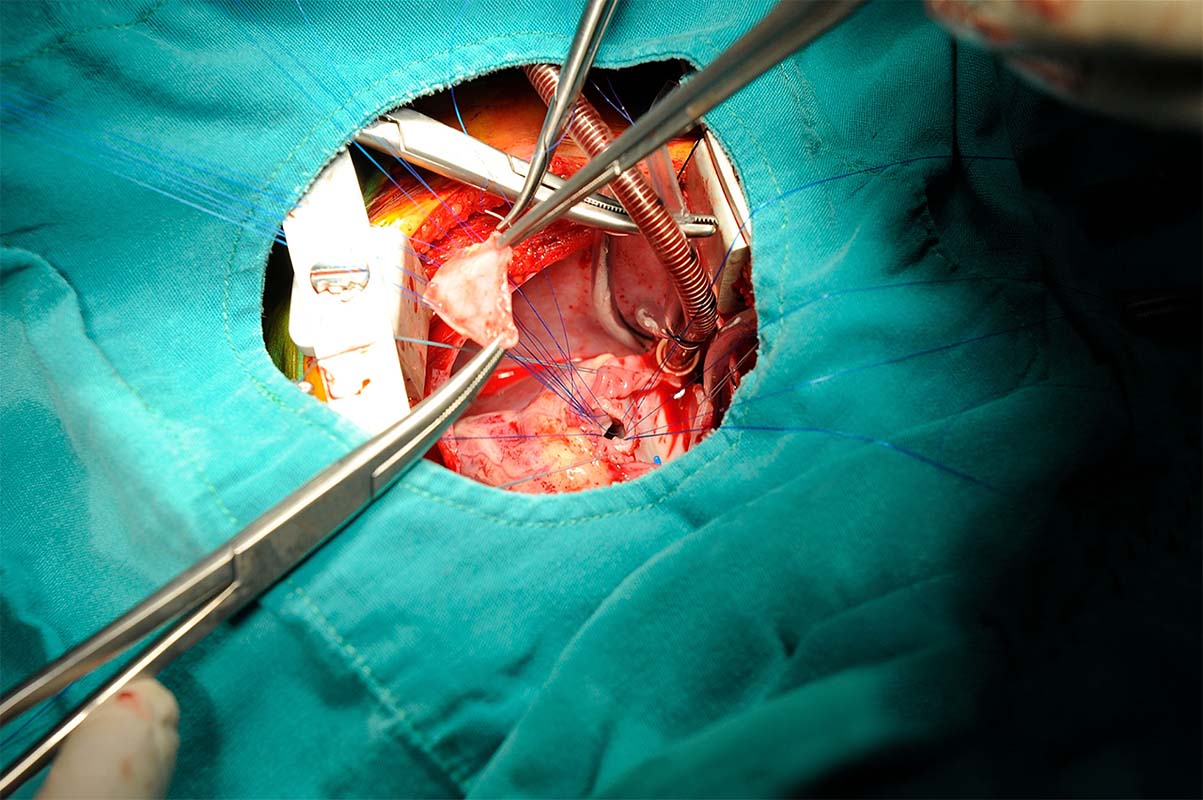
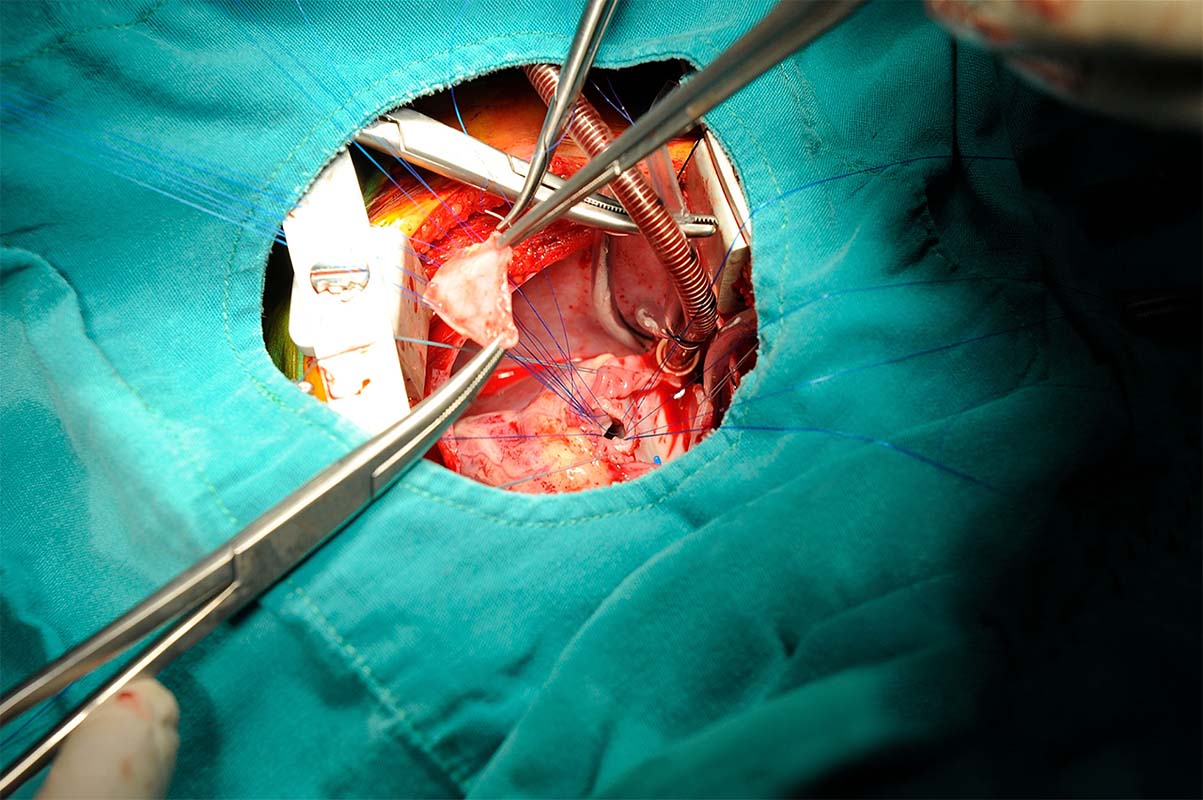
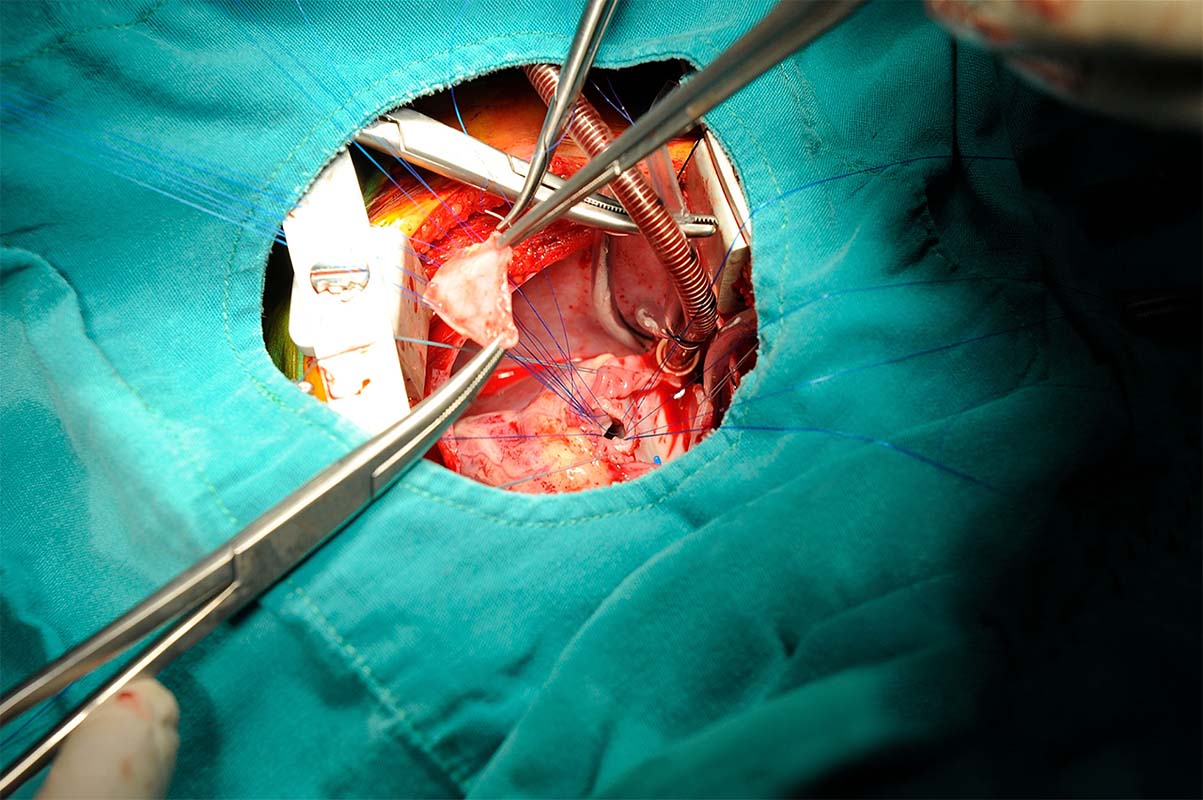
These…life-sustaining innovative therapies that require an ethical framework for shared decision-making with families and medical teams. We suggest a way of structuring team education to benefit urgent ECLS decisions for newborns with moderate to severe hypoxic ischemic encephalopathy (HIE).

Doctors revise their diagnostic strategy to provide a timely and meaningful prognosis in accordance with parental goals. This narrative discusses issues of diagnostic uncertainty and the value of relying on clinical gestalt when trying to prioritize medical tests for a sick patient.