There is no excerpt because this is a protected post.
There is no excerpt because this is a protected post.
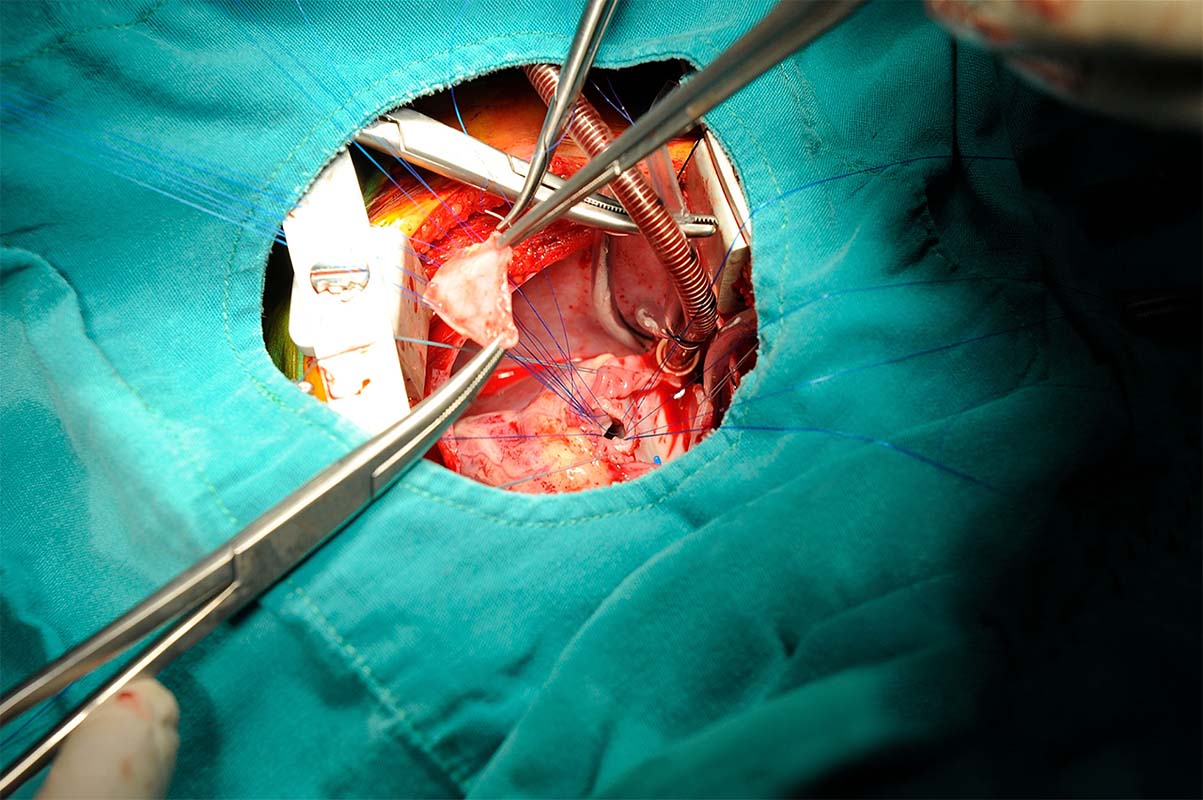
“Suffering” is a concept that is frequently invoked in discussions about medical decision-making in pediatrics. However, empirical accounts of how the term is used are lacking, creating confusion about the concept and leaving parents and providers unsure about the appropriate ways to account for it in pediatric decision-making. We conducted a qualitative content analysis of pediatric bioethics and clinical literature in selected journals from 2007 to 2017 to determine how authors define and operationalize the term when referring to issues in pediatric treatment.

Use of sedation and restraints is sometimes the only means available to stabilize medically fragile eating disorders patients. While minors are not given the option to refuse care that competent adults are, forced tube feeding nonetheless challenges the minor patient’s senses of identity and control. The following case study chronicles the management of an 11-year-old patient transferred from inpatient child psychiatry unit to the adolescent medicine service for nutritional rehabilitation.

This paper presents guidance developed by a multidisciplinary group of bioethicists and patient advocates considering patient- and parent-centric approaches to informed consent in neonatal research in the context of an ongoing clinical trial for neonates with spinal muscular atrophy (SMA).

These…life-sustaining innovative therapies that require an ethical framework for shared decision-making with families and medical teams. We suggest a way of structuring team education to benefit urgent ECLS decisions for newborns with moderate to severe hypoxic ischemic encephalopathy (HIE).
Care providers of critically ill pediatric patients encounter ethically complex and morally distressing situations in their practice. This study sought to identify whether providers remark on ethical conflicts or note moral distress following recent in hospital pediatric death.

The decision to discuss sudden unexplained death in epilepsy (SUDEP) presents a complicated ethical picture with potentially conflicting principles. The neurologist must decide how to disclose and discuss the problem of SUDEP, balancing the desire to help families by empowering them, without doing harm by overwhelming them with fear.
The issue of drug shortages can be framed as those who wish to ensure drug availability in virtue of dedication to the patients’ interests, on one hand, and those who herald economic responsibilities, on the other. A historical and philosophical account of the problem.