White Space
Matthew S. Alexander, Erica M. Carlisle
White Space
ABSTRACT
Evidence-based medicine is a clinical decision-making philosophy that incorporates patient values, best available data, and physician judgment. Information technology in the 21st century has allowed data to become more easily accessed and implemented into clinical practice thus setting a higher expectation for data-driven practice. As a result, the role of physician judgment in clinical decision making has been suppressed, and evidence-based decision-making has evolved into data-driven decision-making—a term used to describe the emphasis on best available data and patient values to the exclusion of physician judgment. However, when clinicians are conditioned to rely on data and suppress clinical judgment, it becomes difficult to manage rare conditions where data is not available. In these circumstances, physician judgment is critical, and clinicians must feel comfortable offering their best clinical judgment to patients and their families. The following discussion recounts one family’s experience with clinical counseling on a rare diagnosis and highlights these arguments.
White Space
White Space
Clinical Vignette
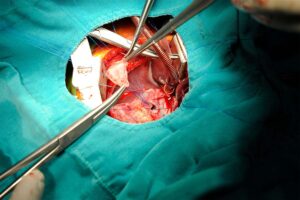
A 30-year-old G1P0 woman presents for her 20-week anatomy scan during a pregnancy that had been progressing normally. The ultrasound was concerning for a complex cardiac anomaly which was confirmed to be a double outlet right ventricle at a 24-week follow-up scan. The patient and her husband received counseling on the diagnosis, and it was explained that as the fetus continued to develop and the heart continued to grow, the approach to managing this complex anatomical defect would likely evolve. A genetic screening in the 30th week was highly suspicious for an extremely rare 6p microdeletion. Only a handful of case reports addressing this unique clinical situation had been published in the literature. Prior to delivery, a multi-disciplinary planning meeting was held to review the most recent echocardiogram and discuss potential medical and surgical plans for the baby following delivery. Participants included the patient, her husband, a neonatal intensivist, a pediatric cardiologist, a social worker, and a care coordinator.
White Space
White Space
White Space
White Space
The soon-to-be parents were well educated, engaged, and had a reasonable understanding of the unpredictability of their child’s cardiac condition. They were aware that a 6p microdeletion added a number of unpredictable variables. Nevertheless, they wanted to discuss the spectrum of possible clinical scenarios so that they could generate an algorithm for how far they would be willing to escalate care. They preferred to think about these scenarios well in advance of delivery to avoid making difficult decisions under intense emotional stress. The patient’s husband wanted to be able to have a thorough discussion with his wife to ensure any decision made for his child would be a joint decision, even in the event of an unforeseen obstetric complication. The couple wanted to prepare themselves for the worst, recognizing they did not want their child to die at a young age with severe intellectual and physical disabilities, all the while battling a cardiac condition that would require repeated operations, hospitalizations, and suffering.
White Space
White Space
White Space
White Space
The soon-to-be parents were well educated, engaged, and had a reasonable understanding of the unpredictability of their child’s cardiac condition. They were aware that a 6p microdeletion added a number of unpredictable variables. Nevertheless, they wanted to discuss the spectrum of possible clinical scenarios so that they could generate an algorithm for how far they would be willing to escalate care. They preferred to think about these scenarios well in advance of delivery to avoid making difficult decisions under intense emotional stress. The patient’s husband wanted to be able to have a thorough discussion with his wife to ensure any decision made for his child would be a joint decision, even in the event of an unforeseen obstetric complication. The couple wanted to prepare themselves for the worst, recognizing they did not want their child to die at a young age with severe intellectual and physical disabilities, all the while battling a cardiac condition that could require repeated operations, hospitalizations, and suffering.
White Space
Discussion
Rare and complicated cases such as this one highlight numerous challenges inherent to clinical decision-making and communication with patients. Medical literature forms the knowledge base for clinical risk assessment and aids providers in sound decision-making. However, when considering rare conditions, clinicians often lack the luxury of established risk scores and clinical pathways. They are instead counseling patients in the realm of clinical uncertainty. This may pose a significant challenge for physicians, especially those who have trained in an era of medicine that places significant focus on data-centric decision-making. In the discussion that follows, we explore how physician dependence on data may result in the omission of physician judgment from clinical counseling.
Physician judgment is often critical in bridging the gap between excellent evidence, or lack thereof, and the individual patient. [1] If physicians are unwilling to exercise their own clinical judgment to make predictions in the absence of data, parents and patients may be confused and unsatisfied with clinical encounters. In short, physician judgment is necessary for good clinical practice because it facilitates decision making in the absence of objective data. That is not to say a physician with good clinical judgment necessarily recommends treatment options. He or she may simply be able to offer insight into what may be expected from a treatment option not well studied, or not well studied in a particular patient.
White Space
Our argument makes use of several terms and concepts that must first be defined. Patient values refers to the compassionate use the individual patients’ predicament, rights and preferences. [2] Best available data refers to clinically relevant research, both from the basic sciences and patient centered clinical research. [2] Physician judgment, or clinical judgment, refers to the acquired proficiencies accumulated by clinicians through experience and clinical practice. [2] Evidence-based medicine is a conscientious, intentional, and calculated medical decision-making philosophy rooted in aforementioned concepts; patient values, best available data, and physician judgment. [3] This triad is uniquely rebalanced and recalibrated with each individual patient to best suit each distinctive clinical situation. [2] Data-driven medicine describes a decision-making philosophy devoid of physician judgment that uses best available research and large retrospective databases to quickly, and in real time, identify patterns and associations in clinical data to generate predictions. [4] The implication being that cognitive biases introduced by clinical judgment can be circumvented by emerging research and powerful tools developed in the information age. [5] An example of data-driven medicine in practice would be using genetic markers to predict whether a patient will suffer an allergic reaction to a particular antibiotic.
Since its initial widespread adoption, the evidence-based medicine triad has colloquially shifted much of its emphasis from physician judgment to best available data. This likely stems from the information boom and the integration of information technology and clinical practice. [6] Today, the term ‘evidence-based medicine’ is sometimes conflated with the idea of ‘data-driven medicine,’ which as noted above, is a decision-making philosophy that relies heavily upon clinical data, patterns, and associations identified by big data, and artificial intelligence—but to the exclusion of physician judgment. [7] Thus, the term ‘evidence-based medicine’ is erroneously applied when clinical judgment is displaced by a dependence on best available data. We worry that data-driven medicine will become the new norm for clinical decision-making. [8]
Physician judgment does not, and should not, supersede best available evidence, but physician judgment remains critical to filling the knowledge gaps in medicine. In the subsequent discussion, we argue that data-driven medicine establishes a clinical decision-making norm that omits physician judgment from clinical counseling. We believe that this is an inadequate approach to clinical counseling that may leave patients confused and unsatisfied, specifically with respect to rare clinical diagnoses where there is insufficient data. Uncertainty will always exist in medicine, and physicians must be comfortable sharing their clinical judgment with patients in these circumstances.
For clinical scenarios in which the disease is common and the evidence is strong, evidence-based medical decision-making and data-driven medical decision-making are quite similar. The evidence based clinical decision-maker recognizes the relatively minimized role of physician judgment in the context of highly dependable data within the evidence-based medicine framework. However, when the disease is rare and the evidence is lacking, evidence-based medical decision-making and data-driven medicine are quite different. The evidence-based medical decision-maker must integrate clinical judgment with patient values. Meanwhile, the data-driven decision-maker, who has been conditioned to resist imposing his/her clinical judgment, may avoid introducing non-validated data into the clinical decision-making calculus, leaving the patient without data and without guidance.
To illustrate these points, consider how the data-driven decision maker and evidence-based decision maker may address the clinical scenario described previously. When prompted about how long the infant would be expected to live and what functional capacity the infant would be expected to have, the data-driven decision maker can make no reasonable estimation because there is insufficient data regarding cardiac anomalies in the context of a 6p microdeletion in the literature. The evidence-based decision-maker, can appeal to their own clinical judgment and make an estimation based on their experience and knowledge.
Regardless of an individual provider’s decision-making style, patient communication and clinical decision-making are tightly linked through patient-centered care. [9] It is the responsibility of the physician to sufficiently educate the patient with complete and accurate information so the patient may make an informed decision. The physician must be cognizant of how the substance and reliability of the information he/she presents influences patient perspectives and guides decision-making. Likewise, a physician must also be aware of how the information or personal insights he/she omits impacts decisions. The evidence-based medicine decision-maker is comfortable including clinical judgment as an educational tool with the caveat that such information is subject to a degree of error commensurate with the level of clinical uncertainty. Alternatively, much like the physicians in the example case, the data-driven decision-maker finds clinical judgment unfit for patient education purposes and may be unwilling to reveal this information even at the request of the patient.
Whether presented in an evidence-based or data-driven framework, most believe that patients generally value shared decision-making. [10] However, it is not known whether this decision-making approach is preferred when data is scarce, the condition is complex, or the patient is a child. [11] Additionally, some studies have suggested that many patients prefer not to be at the center of medical decision-making. [12,13,14] Rather, many patients prefer to have insight offered by their physician, and some patients even consider this guidance to be the most important information they use to develop their own opinion. [1] Despite this, many physicians seem unwilling to share their recommendations with patients, even when directly asked (i.e. “What would you do if this were your partner/parent/child?”) Perhaps this reticence to offer guidance serves to guard physicians against the potential vulnerability caused by exposing their opinions or intuition.
One may question whether the physician has not just an option, but rather an obligation to offer a clear recommendation in clinical settings in which the condition is rare and the evidence is lacking. In such settings, physician judgment may be viewed as a medical resource that has been developed over years of education, training, and experience. One may thus argue that this carefully cultivated product ought not be denied to the patient. Further, one may suggest that clinical judgment is critical for the good practice of medicine, thus a physician’s fiduciary duty to a patient ethically and professionally obliges him or her to offer clinical judgment. Conversely, one may argue that providing physician judgment may minimize respect for patient autonomy and result in coercion. However, it seems that physician judgement could be thoughtfully included in clinical counseling in an instructive, but non-coercive manner, such that respect for patient autonomy is promoted.
Evidence-based medicine and patient-centered care are cornerstones of modern Western medicine. However, the displacement of evidence-based medicine by data-driven medicine has created new normative biases in medical decision-making and patient communication that are at odds with patient-centered care in the context of rare conditions. Lantos describes this as an “objective information” approach to decision making whereby the physician is merely a facilitator of information, providing only the facts necessary for patients and families to make their own health care decisions. [15] However, the expectation that patients can participate in their own clinical decision-making in this way, when there is little prognostic data available and the physician is not willing to estimate a prognosis based on his or her own clinical judgment, seems inherently flawed and unrealistic.
This challenge will likely not be solved with a reductionist approach to medicine. Even as scientists gain more insight into the genetic and molecular mechanisms of disease, and treatments and therapies are improved, knowledge can never be complete. [16] Patients will become more complex and new uncertainties will emerge [17] —a cycle likely to persist indefinitely.
Thus, we cannot depend on the expansion of evidence-based medicine to eliminate medical uncertainty and shield physicians from the responsibility of formulating and sharing clinical judgment. Physician judgment is a sacred domain that will be inhabited by the medical profession for the foreseeable future. Physicians should be good stewards of this valuable tool. It is inappropriate to withhold this tool from patients. The fiduciary duty of a physician to his or her patients as well as the ethical principles of beneficence and non-maleficence mandate that patients are entitled to physician judgment as part of the patient-physician covenant, and when shared responsibly and appropriately, physician judgment can build trust and strengthen relationships between patients and physicians.
White Space
Case Conclusion
The family in the case scenario presented at the outset of this article sought a second opinion at another tertiary care center. The family elected to transition their care to that team. Ultimately, they felt more comfortable with the experience level in neonatal complex cardiac care of the team offering the second opinion. Much like the first care team, the second care team was unable to offer specific predictions based on data, but they were willing to provide critical insight with rough estimations based on their experience with similarly complex cases. After this discussion, the family felt comfortable proceeding with surgery.
The infant underwent successful operative repair of the congenital cardiac defect on day-of-life eight. No further cardiac surgeries are anticipated until adulthood and activity limitations based on cardiac function are expected to be minimal. Several additional minor surgeries were required during the first year of life to manage a variety of non-life-threatening urologic and auditory anomalies. Cognitive developmental delays are expected but the full extent remains unknown at this time due to the variable penetrance of the genetic condition.
White Space
White Space
The authors have disclosed no conflicts of interest.

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
White Space
White Space
Affiliations
Matthew S. Alexander, MD MHA1
Erica M. Carlisle, MD1,2
- Department of Surgery, University of Iowa Hospitals and Clinics, Iowa City, Iowa
- Program in Bioethics and Humanities, University of Iowa Carver College of Medicine, Iowa City, Iowa
Correspondence
Erica M. Carlisle, MD
Assistant Professor of Surgery
University of Iowa
200 Hawkins Drive 2966-Z-JPP
Iowa City, IA 52242
[email protected]
White Space
White Space
Endnotes
1. Stiller K. It’s not the evidence, it’s the way you use it: is clinical practice being tyrannised by evidence? My experience with the PBAC and evidence-based practice. Aust. Health Rev. May 2008;32(2):204-207. https://www.researchgate.net/publication/5404265_It’s_not_the_evidence_it’s_the_way_you_use_it_is_clinical_practice_being_tyrannised_by_evidence_My_experience_with_the_PBAC_and_evidence-based_practice
2. Sackett DL, Rosenburg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. BMJ. 1996; 312(7023): 71-72. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2349778/?page=1
3. Masic I, Miokovic M, Muhamedagic B. Evidence based medicine–new approaches and challenges. Acta Inform Med. 2008; 16(4): 219-225. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3789163/
4. Mitchum, Rob. “Data-Driven Medicine.” UChicago Medicine – At The Forefront, UChicago Medicine, 24 Apr. 2017. www.uchicagomedicine.org/research-and-discoveries-articles/data-driven-medicine.
5. Shah NH, Tenenbaum JD. The coming age of data-driven medicine: translational bioinformatics’ next frontier. Journal of the American Medical Informatics Association: JAMIA. 03/26/accepted 2012; 19(e1): e2-e4. https://www.ncbi.nlm.nih.gov/pubmed/22718035
6. Straus SE, McAlister FA. Evidence-based medicine: a commentary on common criticisms. CMAJ. 2000;163(7):837-841.
7. Rowley, Robert, et al. The relationship between evidence-based and data-driven medicine. CIO, CIO, 25 Oct. 2017. www.cio.com/article/3235025/healthcare/the-relationship-between-evidence-based-and-data-driven-medicine.html
8. McCue ME, McCoy AM. The scope of big data in one medicine: unprecedented opportunities and challenges. Front Vet Sci. 11/16 2017;4:194.
9. Constand MK, MacDermid JC, Dal Bello-Haas V, Law M. Scoping review of patient-centered care approaches in healthcare. BMC Health Serv Res. 2014; 14: 271-271. https://www.ncbi.nlm.nih.gov/pubmed/24947822
10. Mazur DJ, Hickam DH. Patients’ preferences for risk disclosure and role in decision making for invasive medical procedures. Journal of General Internal Medicine. Feb 1997; 12(2): 114-117. https://www.ncbi.nlm.nih.gov/pubmed/9051561
11. Carlisle EM, Shinkunas LA, Kaldjian LC. Do surgeons and patients/parents value shared decision-making in pediatric surgery? A systematic review. Journal of Surgical Research. Nov 1 2018; 231: 49-53. http://www.asc-abstracts.org/abs2018/47-13-do-surgeons-and-patients-value-shared-decision-making-in-pediatric-surgery/
12. Strull WM, Lo B, Charles G. Do patients want to participate in medical decision-making? JAMA. Dec 7, 1984; 252(21): 2990-2994. https://www.ncbi.nlm.nih.gov/pubmed/6502860
13. Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision-making. A national study of public preferences. Journal of General Internal Medicine. Jun 2005; 20(6): 531-535. https://www.ncbi.nlm.nih.gov/pubmed/15987329
14. Robinson A, Thomson R. Variability in patient preferences for participating in medical decision-making: implication for the use of decision support tools. Quality in Health Care: QHC. Sep 2001; 10 Suppl. 1: i34-38. https://www.ncbi.nlm.nih.gov/pubmed/11533436
15. Lantos, J. D. (2008). Neonatal Bioethics: The Moral Challenges of Medical Innovation. The Johns Hopkins University Press. Baltimore, MD 113-121
16. Hubbard R, Wald E. Exploding the Gene Myth: How Genetic Information Is Produced and Manipulated by Scientists, Physicians, Employers, Insurance Companies, Educators, and Law Enforcers; with a New Afterword. Beacon Press; 1997.
17. Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet 2015;386(9995):743-800. doi: 10.1016/S0140-6736(15)60692-4. Epub 2015 Jun 7 https://www.ncbi.nlm.nih.gov/pubmed/26063472