Ethical Stress, Virtues and Values Conflict in Pediatric Death
Stephanie Kukora, Naomi Laventhal, Patricia Keefer, Janice Firn
ABSTRACT
Background: Care providers of critically ill pediatric patients encounter ethically complex and morally distressing situations in their practice. Though many providers receive an introduction to ethics during training, their retention and application of ethical principles to daily clinical practice may be limited. Furthermore, current approaches to clinical ethics consultation focus on specific problems of individual patients, and may not meet the emotional and debriefing needs of providers.
Objectives: To identify whether providers remark on ethical conflicts or note moral distress without being specifically prompted, when asked to share thoughts, comments, questions about a recent in hospital pediatric death, and to characterize the nature of these conflicts and distress.
Methods: Constructivist thematic analysis of survey free-text responses from providers involved in a deceased patient’s care in the 24 hours prior to the patient’s death.
Results: There were 307 (35%) free-text responses in 879 completed surveys (33% total response rate), regarding the deaths of 138 pediatric patients (81% of in-hospital pediatric deaths that occurred) between November 2014 and May 2016. Diverse provider roles were represented, and patients died in multiple hospital units. Two main themes were identified: Ethical issues addressed with traditional ethics education, and ethical issues not addressed with traditional ethics education, which consisted of two sub-themes: virtue conflicts and value conflicts.
Discussion/Conclusion: Many providers experience ethical conflicts with pediatric end of life care but may not be able or willing to share these candidly. Targeted education to assist hospital staff in identifying and resolving ethical conflicts encountered in pediatric end-of-life care, and further ethical support for providers to share or debrief safely, without criticism or negative repercussions, may be warranted.
Background
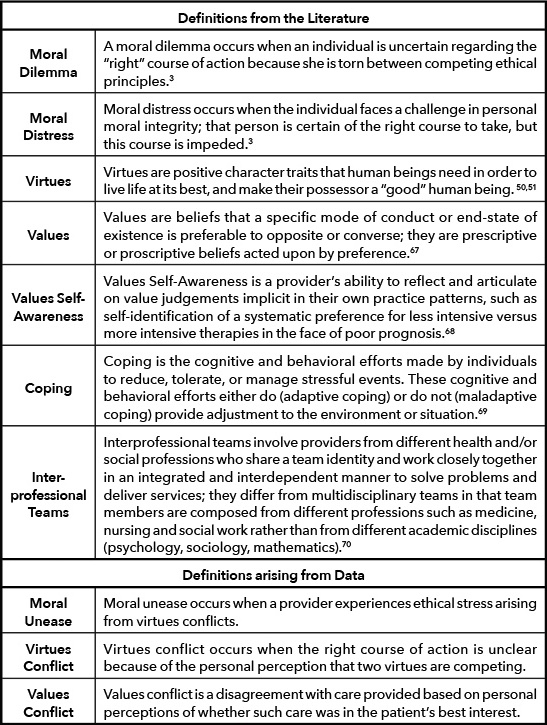
Ethically challenging situations arise in providing care for critically ill and dying patients. [1] While death occurs far less frequently among neonatal and pediatric patients than adult patients, the emotional impact of witnessing the death of a patient is greatly amplified if that patient is an infant or child. [2] Providers who participate in caring for these patients and their families may suffer psychological harm stemming from moral dilemmas and distress (Table 1). [3] The consequences of repeated exposure to these types of ethical stressors can lead to significant burnout [4,5] and compassion fatigue [5,6], affecting not only the mental health of the provider, but also compromising the care they give to patients. [7]
Hospital Institutional Ethics Committees (IECs) provide ethics support at an institutional level, and should, in principle, reinforce basic ethics education provided in most training programs for health professions. Their role includes resolving conflicts surrounding patient treatment decisions through clinical case consultation, offering a forum for discussion of policies involving institutional ethics, and providing education about ethical concepts to their health care communities. [8] Though requesting clinical ethics consultation is encouraged for any patient, family member, or provider on the care team who is perplexed by an ethically complicated scenario, not all such cases are examined by formal clinical consultation. In the pediatric population, ethics consultations are often called for cases with prolonged hospitalizations or illness, particularly when values differences exist between the patient/family and medical team. [9,10,11,12] Patients with acute clinical worsening or unexpected death, resulting in shorter duration of illness or hospitalization may create ethical stress but not receive formal ethics consultation for practical reasons. For example, a pediatric patient arriving to the emergency department may die following a prolonged resuscitation attempt and cause providers to raise ethical questions about whether heroic interventions were in the patient’s best interest or merely caused suffering. Such a brief course and subsequent demise, however, would likely prohibit sufficient opportunity for the ethics committee to be consulted and provide recommendations on ethical decision-making in this context.
Similarly, cases in which values differences occur amongst providers on the medical team, rather than between the team and patient/family, also cause ethical distress but may not always be raised to the level of formal ethics consultation. [13] Providers with lower hierarchical privilege, particularly nurses, may be reluctant to or face repercussions for requesting clinical ethics consultation. [14] Education and empowerment of these providers is likely insufficient to overcome the systematic barriers that impede them from requesting clinical ethics consultation as a tactic to mitigate their distress. [15]
When consulted, IECs advise clinical care teams regarding the ethical permissibility of possible care options and assist in identification of value conflicts in the setting of a specific patient or scenario. Traditional consultation models rely on medical providers, patients, or patient surrogates/family members advocating for the patient requesting IEC involvement. However, this excludes cases not identified as warranting consultation. This model is not well suited to address general concerns by teams or individuals about recurring ethical issues, or to offer a forum for staff experiencing personal moral distress, [16,17] particularly those with lower hierarchical privilege on the team. Traditional ethics education focusing on knowledge and application of bioethical principles to resolve conflicts does not address personal ethical struggles, such as values conflicts and moral distress. [18]
Providers may receive an introduction to clinical ethics during their training, however, limited clinical experience may hinder their ability to integrate this information and apply it to daily practice. [19] Though IECs are tasked with the responsibility of ethics education for hospitals, current guidelines do not recommend strategies for imparting role-specific ethical knowledge to providers. [8] Additionally, debate exists regarding how to ensure appropriate understanding and situational application of ethical concepts to all providers within a healthcare system. [20–29] Although moral distress is a specific focus of increasing empirical investigation, particularly among inpatient hospital nurses, [16–18] the effectiveness and impact of routine, training-program-based ethics education, as well as IEC provided ethics education, is not well informed by empirical evidence. Little is known about the nature and frequency of ethical stress encountered by interprofessional (Table 1) health care providers in the care of dying children, as many of these cases, for the reasons noted above, do not rise to the level of IEC involvement.
Survey studies have sought to quantify and characterize the frequency and severity of moral distress experienced by providers caring for critically ill and dying infants and children. [30–33] Others have correlated moral distress with knowledge of guidelines [34] and outcomes. [35] Several qualitative studies [36–43] have explored ethical issues related to pediatric death but are limited by a small sample size, few include inter-professional providers [36,38,40], and most have asked providers to recall a clinical situation of their choice in which they experienced moral distress/challenging situations [36–39] or cared for a dying patient. [41,42] Few have examined whether respondents comment on ethical issues without specific prompting [40,43] only one has inquired about individual patient deaths. [40]
To increase the body of evidence around the incidence moral distress among care providers, we sought to identify whether providers described ethical conflicts or note moral distress without being specifically prompted to do so, when invited to share thoughts and/or comments about the recent in-hospital death of a pediatric patient for whom they personally provided care in the preceding 24 hours. We also aimed to characterize the nature of these conflicts and distress if found, to further inform targeted ethics education and clinical support for interprofessional healthcare providers of pediatric end-of-life care, based on ethics-related provider experiences at the bedside of dying children.

Nearly one-quarter of respondents described experiences of ethical distress following the death of a patient, and much of what was described was not addressed by traditional ethics education, suggesting the use of targeted education, perhaps through preventitive ethics rounds or narrative ethics techniques.
Methods
Constructivist thematic analysis of free-text survey responses was used to explore whether providers remarked on ethical conflicts or noted moral distress without prompting after the death of a patient for whom they had provided care. This project was exempt from review by the Michigan Medicine institutional review board (HUM00116059) as part of an ongoing quality improvement effort.
Sample and Recruitment
Survey respondents were interprofessional care providers at a 348-bed pediatric academic medical center in the state of Michigan. All providers (n=2701) who cared for a patient less than 18 years of age within the 24-hour period leading up to his or her death were identified via the electronic medical record. Participation was voluntary; responses were anonymous as to specific participant identity, although the survey did request information about role on the provider team and unit in which care was provided.
Data Collection
An electronic survey via Qualtrics [44] software was emailed to each provider within one week of the death between October 2014 and May of 2016. The survey, developed by the institutional Pediatric Palliative Care Team, requested demographic information, information about the case, whether the death occurred following active resuscitation efforts or comfort care, provider role and unit, and provider level training and years of professional experience. A free-text response box was provided at the conclusion of the survey, inviting participants to “share thoughts, comments, or questions” about their experience with that particular patient’s death, but did not specifically inquire about ethical stress. Prior to distribution, the survey was reviewed for face and content validity, and was piloted for feasibility. No changes were made to the survey following a successful pilot study.
Analysis
De-identified quantitative survey response data were imported into Excel (PK) and descriptive statistics were completed (SK). Free text responses were analyzed and tracked in Dedoose [45] to enhance trustworthiness and credibility of the data. [46,47] Inductive, constructivist thematic analysis with line by line coding [41] was performed by SK, who developed the codes and themes in discussion with JF, PK, NL using an iterative process to challenge identified themes, and allow for on-going reconceptualization of themes. A constructivist approach “assumes the relativism of multiple social realities, recognizes the mutual creation of knowledge by the viewer and viewed, and aims toward an interpretive understanding of participants’ meanings.” [48] Throughout the process reflexivity was used to challenge preconceived ideas and enhance rigor. [49] Themes were considered robust when coherent, consistent, and distinctive.[49]
Results
Participant Characteristics
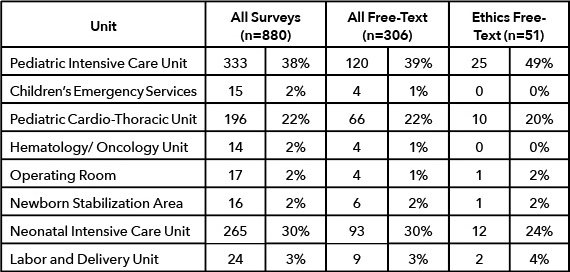
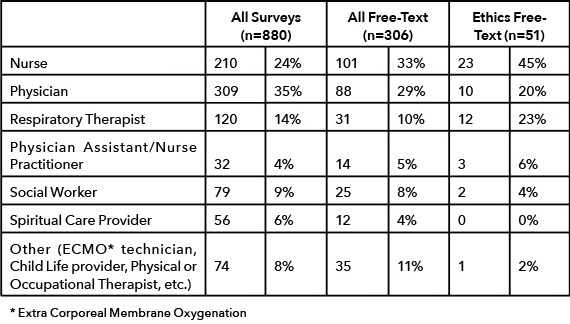
There were 880 surveys completed out of 2701 emailed to providers identified by the medical record as having participated in a pediatric patient’s care in the 24 hours preceding that patient’s death (33% total response rate). At least one completed survey was returned for 167 of the 168 deaths occurring between November 2014 and May 2016 (99.4% of deaths). There were 306 (35% of completed surveys) free-text responses, and at least one free text comment was made regarding the deaths of 138 pediatric patients (81% of in-hospital pediatric deaths that occurred in that time period). Fifty-two respondents described ethical challenges surrounding their patients’ deaths, corresponding to 17% of those providing free-text responses and 6% of all survey respondents. Comments regarding ethical conflict were identified for 38 unique patient deaths (23% of all pediatric deaths) with 2 patients receiving comments from 3 individuals and 8 receiving comments from two. Diverse provider roles were represented (Table 2), caring for patients who died in multiple hospital units (Table 3).
Themes
Constructivist thematic analysis identified two main themes: Ethical issues addressed with traditional ethics education and ethical issues not addressed with traditional ethics education, which consisted of two sub-themes, virtue conflicts and value conflicts. Themes are described below supported by quotations (Tables 4,5,6).
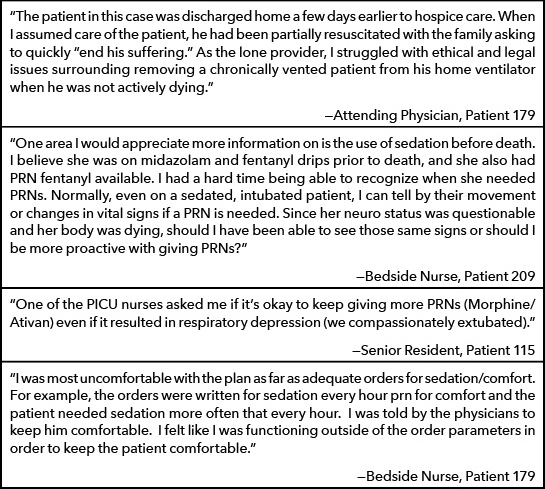
Ethical Issues Addressed with Traditional Ethics Education (Table 4)
A number of respondents discussed personal ethical struggles pertaining to their role as a provider in the patient’s end-of-life care. One described concerns about their own moral culpability in discontinuing life-sustaining interventions in a patient whose condition was stable on these care modalities. This respondent expressed discomfort with uncertainty of outcomes/prognosis, including futility, and the gravity of making irreversible decisions, but did not indicate that such a course of action was in conflict with their personal values. Similarly, multiple respondents expressed concerns about inadvertently hastening the patient’s death when administering medications intended to alleviate suffering.
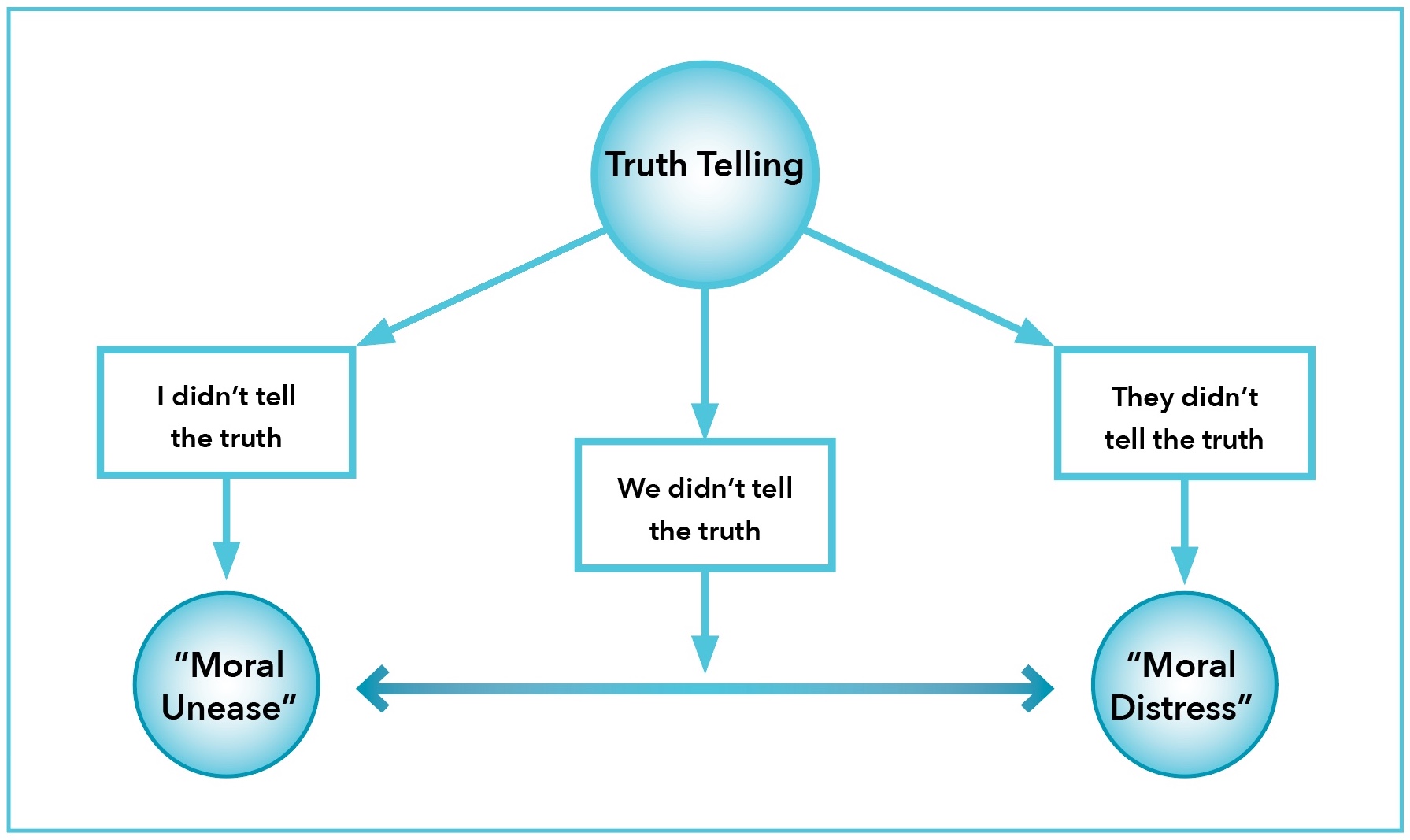
Ethical Issues Not Addressed with Traditional Ethics Education: Virtues Conflicts (Figure 1)
Respondents also described ethical struggles involving virtues conflicts, specifically honesty versus compassion when it comes to truth-telling with families at the end of life. Virtues are positive character traits that makes their possessor a “good” human being, but at times, two or more virtues may oppose or contradict each other (Table 1). [50,51] Experiences with truth-telling varied with the perceived level of personal responsibility on the part of the respondent. We sub-categorized these by whether the responsibility to be truthful belonged to other members of the care team (They Didn’t Tell the Truth), belonged exclusively to the respondent (I Didn’t Tell the Truth), or was shared between the respondent and others (We Didn’t Tell the Truth, Figure 1). Respondents who did not have authority about what was communicated reported ethical tension with their roles in the patient’s care which is consistent with traditional moral distress [3] their discomfort arose from being complicit with an action they found morally wrong but were unable to correct. Other respondents, who felt personal responsibility for the communication, chose not to be truthful in their situations despite having the ability to take this course of action and expressed feeling troubled by their choice. We identified this phenomenon as “moral unease.”
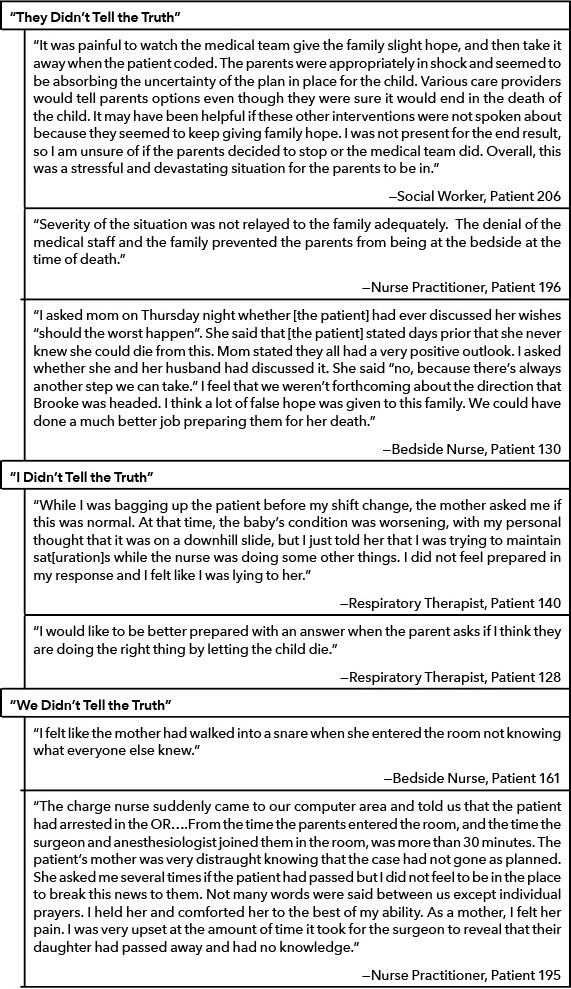
They Didn’t Tell the Truth: Honesty as a team, without personal responsibility (Table 5)
Several respondents described situations in which they perceived other members of the care team not being honest with the family, particularly regarding a poor prognosis or likely death of a child. In these responses, respondents reported ethical conflict consistent with moral distress, as they felt that something morally “wrong” was happening, but felt unable to personally rectify the situation. Often these responses correlated truth-telling with its effect on patient care. Respondents noted that others’ failure to be honest negatively impacted the quality of the patients’ death by delaying provision of comfort measures, or deterring parents’ presence at the bedside. No responses described failure to tell the truth by other members of the care team as being compassionate or having a positive impact on the patient’s death.
I Didn’t Tell the Truth: Honesty as an individual provider (Table 5)
Several respondents noted that while providing end-of-life care they had not been honest when speaking to families. Some felt uncomfortable engaging in a conversation about a child’s worsening clinical condition. Though it is possible this discomfort stemmed from lack of experience in having difficult conversations, or hierarchical considerations in which they did not feel that the disclosure of bad news was within their purview, it seemed, at least in part, these respondents chose to withhold information when they had the ability to be truthful. In these responses, the decision to withhold information seemed to be made in an effort to be compassionate to the family of the dying child. When ethical stress about personal responsibility in truth-telling was present, multiple respondents described feeling “unprepared” to answer questions posed by the patients’ families, suggesting difficulty navigating ethically stressful situations based on virtues conflicts, struggling to reconcile their perceived inability to be both truthful and compassionate in these end-of-life scenarios.
We Didn’t Tell the Truth: Shared personal responsibility of an individual as part of the team (Table 5)
Some of the responses described clinical scenarios in which the respondent shared personal responsibility for truth-telling with other care providers on the team, but that the truth was not honestly disclosed by any care team member. These responses portrayed the experiences negatively, and noted feeling “sneaky” and “underhanded,” or having the perception of collusion between care-team members. A few respondents described withholding the truth as a burdensome experience; they reported that being part of the team knowing something the family did not know trapped them into keeping a secret. Like those who individually had not been truthful, these respondents had the ability to be honest with families; they chose not to do so, and expressed ethical stress in these encounters. There was an additional component of moral distress in two scenarios: those who felt powerless to divulge information to families, as it was not appropriate given their role on the care team, and those that did not have the information necessary to be fully honest.
Ethical Issues Not Addressed with Traditional Ethics Education: Values Conflicts
Many respondents described ethical distress surrounding the death of their pediatric patient stemming from values conflicts about the goals and level of care provided. Ethical shared decision-making supports that in situations of uncertainty, such as end-of-life care provision, medical decisions should be based on the patient’s or family’s values, not personal values of the providers. [52] In all cases in which a values conflict was described, respondents expressed an opinion that care was inappropriately aggressive at the end-of-life (Table 6). There were no responses in which respondents lamented that they were ethically distressed by having to be complicit in a premature transition to comfort goals that was maligned with their personal values.
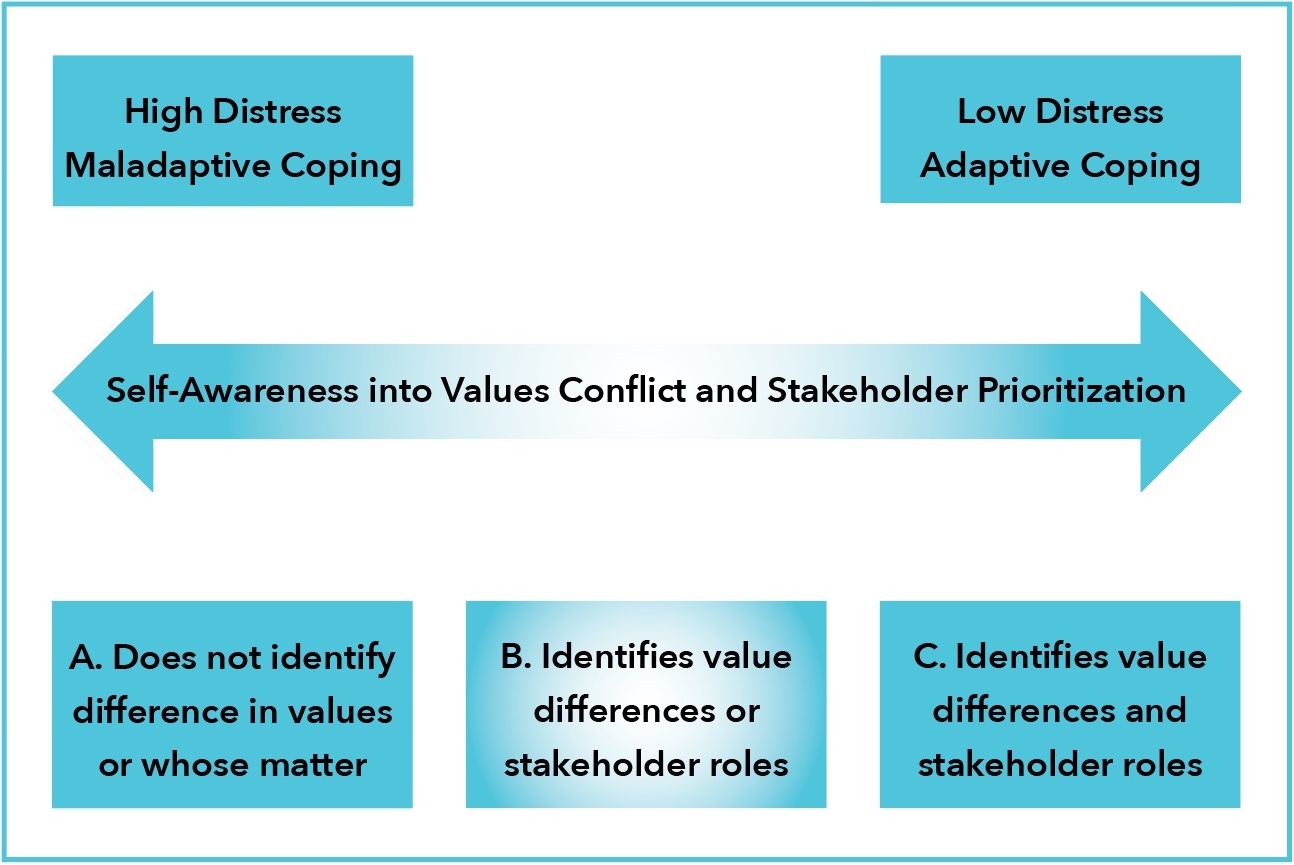
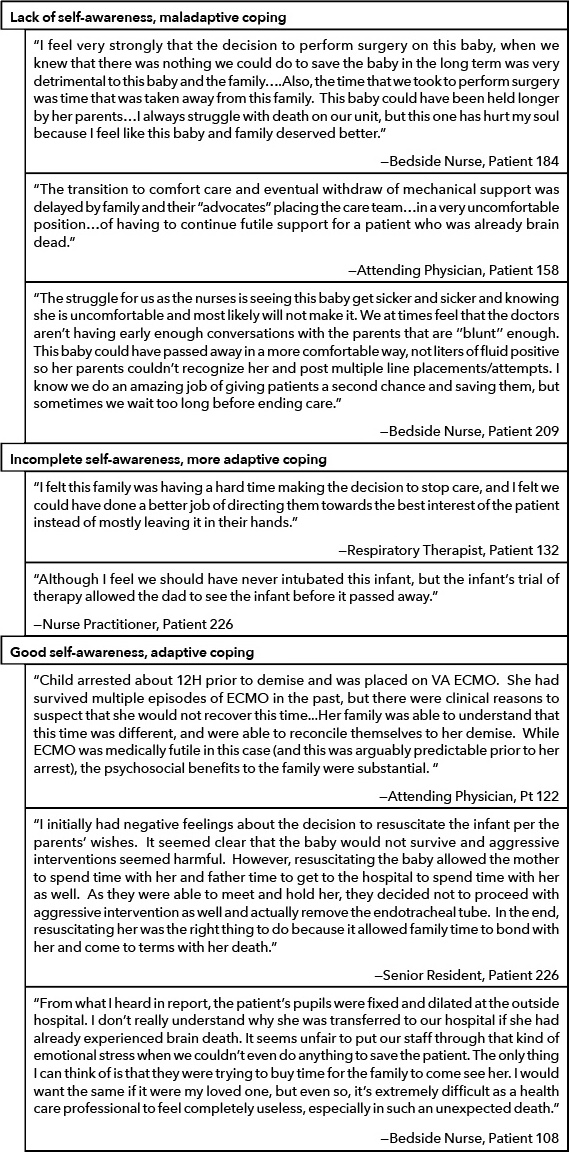
Responses depicting values conflicts fell across a spectrum, with poor self-awareness into the nature of the values conflict or poor/incomplete identification of stakeholders correlating with maladaptive coping (Figure 2), and good self-awareness (Table 1) and identification of these determinants correlating with adaptive coping (Figure 2).
In responses which described values conflicts without identifying the source of distress, respondents voiced their disagreement with interventions that they did not believe conveyed therapeutic benefit to the patient, but failed to acknowledge that there may be differences in opinion regarding the futility of these interventions (Figure 2 Box A). Likewise, they did not identify that other stakeholders, including other care team members, and especially parents, may have had differing, valid opinions on care goals, and that decision-making should be more strongly influenced by these opinions instead of their own. Strong emotional language in these responses emphasized the deep, personal impact that the perceived inappropriate care had on these respondents (Table 6). Other responses demonstrated some, but incomplete, self-awareness into the values conflicts underlying their ethical stress (Figure 2 Box B). These respondents identified that they were faced with an ethical issue, and/or identified that values differences existed, but did not accurately acknowledge whose values should have been given precedence in decision-making (Table 6). Finally, there were respondents who identified values differences and appropriately identified the priority of stakeholder values in decision-making (Figure 2 Box C). These responses often contained indicators of adaptive coping and acceptance of the outcome (Table 6).
Discussion
To our knowledge, our study of unprompted free-text survey responses is the first to empirically study the incidence of moral distress and ethical conflicts in end-of-life care for specific pediatric patients by interprofessional providers. Many interprofessional providers experience ethical conflicts with pediatric end-of-life care but may not be willing, or have opportunity, to share their concerns candidly. Though comments specifically describing ethical stress were provided by a minority of survey respondents, more than one quarter of the deaths in this time period had at least one provider comment on an ethical issue encountered in providing end-of-life care for that patient. These findings are consistent with previous survey and qualitative studies that note ethical stress occurs in these clinical situations, but not with overwhelming frequency. [30–33]
Our findings expand on the growing body of evidence around the incidence of moral distress among care providers in two important ways. First, this study quantifies the incidence of provider-focused ethical phenomena within an interprofessional care team; second, it offers novel and informative categorization of ethics-related provider experiences at the bedside of dying children.
Responses described several types of ethical stress, some of which are addressed in current models of ethics education[20–29] focusing on applications of bioethical principles and knowledge of pertinent guidelines. Previous studies have demonstrated these situations are distressing to providers, and that knowledge deficits of existing guidelines are contributory. [34] Only a few respondents described scenarios of common ethical conflicts for which clear ethical guidance exists. This finding suggests that our current educational efforts to empower providers, as well as ethics committee support, have likely aided most providers in ethically challenging situations that have precedence set for how to resolve them. While profession-specific ethics education exists, and limited interprofessional classroom ethics courses are available to some, expansion of existing ethics education models to include interprofessional providers in the clinical setting is vital, as unaddressed ethical issues negatively affect patients, families, and providers. [53–56]
The classroom setting alone is insufficient to meet this need as learners often struggle to apply classroom knowledge to problems in the clinical setting; [24] ethics education is most effective when is tailored to the inter-professional teams’ education needs within the clinical context. [57–59] One mechanism that may allow for real-time embedded interprofessional ethics education within the clinical setting is the concept of preventative ethics rounds. [29,60] Preventative ethics rounds serve to help interprofessional teams anticipate, navigate and mitigate potential ethical conflicts and tensions before they become crises, necessitating formal ethics consultation; they do so by:
- Providing support for specific patient care situations
- Giving a space for interprofessional team members to better understand each other’s professional obligations, and
- Providing a space for education in moral reasoning and engaging in reflective practice. [23,25,29,60,61]
In our study, we also identified two sources of ethical stress that could be positively impacted from a preventative ethics approach. First, respondents specifically revealed ethical stress in experiences surrounding truth telling. Interestingly, when respondents perceived other members of the medical team were not honest, they identified this non-disclosure of truth as harmful to the patient/family. When respondents reported ethical stress about not being truthful themselves, however, it appeared that they were struggling to find a balance between being honest and being compassionate. We specifically identify this ethical stress as arising from virtues conflict (Table 1). Though from the responses it appears these providers concluded that in their specific situations disclosure of the truth would have been more harmful than beneficial, the experience of being untruthful was distressing, and they commented about it without being prompted. The cause of this disparity in how respondents perceive truth telling based on their role and responsibility in the situation is unclear. Whether it stems from differences in the type or importance of information being withheld, or difficulty with perspective taking by the provider to understand that others who do not disclose the truth may be experiencing virtues conflict, was not discernible from the comments; we think this deserves further investigation. Likewise, ethical stress experienced by providers arising from virtues conflicts, which we have termed “moral unease,” to facilitate further study, has not been well characterized in the literature, though we think that this phenomenon warrants further scrutiny to determine its impact on compassion fatigue and burnout among providers.
Current models of ethics education describe the importance of a provider being honest as key to facilitating patient autonomy. These are grounded in the premise that honest disclosure of medical information, supports patients making informed decisions about their health. While being truthful in the medical context is often consistent with the ethical course of action, there may be specific situations in which disclosure of truth might be harmful. An approach to ethics education that imparts moral reasoning may guide providers in how to deliver difficult information honestly and compassionately, such as weighing the dangers of not being truthful (personal virtues compromise, potential breach of trust with parents) against those of telling the truth (upsetting fragile parents, not being able to give whole story, breaking trust of team). Novel education approaches, such as team simulation exercises and use of structured debriefs [29] following sensitive or difficult discussions might be helpful to strengthening providers’ skills in the domain of truth telling. Narrative medicine, which has been proposed as a model for imparting empathy, reflection, and professionalism to medical providers, [62] may also serve a role in assisting providers in growing in self-awareness, gaining perspective, and navigating complex situations surrounding truth-telling in pediatric end-of-life care.
Second, values conflicts (Table 1) accounted for most of the ethical stress reported. Our findings are similar to previous studies which have noted that providers perceive care decisions at end-of-life to be more aggressive than they believe is in the child’s best interest. [40–42] Our study results offer a more structured framework with which to analyze values differences. We noted varying levels of self-awareness in respondents’ understanding that values differences were the source of their distress. Individuals who appeared to be better at identifying values differences exemplified more adaptive coping. Respondents who did not identify the presence of values conflict often attributed medical decision-making with which they did not agree to failure of physicians to educate families. The assumption that no adequately informed parent would make choices differing from their own often resulted in misclassification of the conflict as a truth-telling failure on the part of others. These individuals used very emotional language in their responses, likely related to moral emotions, or the guilt, anger, resentment, or indignation an individual’s experience when they perceive that they or someone they care about has been wronged, offended, slighted, or harmed. [63] Though the respondents in these situations may not have accurately assessed the medical situation or context for decision-making, their narrative is influenced by this perspective. Conflicts arising from these values differences cannot be resolved without acknowledgment of the providers’ experience and perspective.
Conclusion
By showing that at least one provider described experiences with ethical distress without being specifically prompted for nearly one quarter of in-hospital pediatric deaths, and that much of the described distress is not often addressed by traditional clinical ethics education, our results suggest that targeted education, such as the use of preventative ethics rounds, or the use of narrative medicine, to assist staff in identifying and resolving ethical conflicts encountered in pediatric end-of-life care may be helpful. Though the ethics committee can assist in resolving moral dilemmas and identifying values conflicts when consulted, consultation might not occur until the situation has deteriorated considerably, and might not occur at all, if there is no clear disagreement between the patient’s parents and the team. Additional approaches to eliciting and assisting all providers on the care team with ethical stress in pediatric end-of-life care should be pursued to address this problem. Team debriefing with an ethics expert after a patients’ death may assist in identifying conflicting values and lead to philosophical discussion on responsibility/roles of stakeholders in healthcare decision-making. Debriefing could also assist providers expanding their perceptions of a complicated medical situation from alternate perspectives to reduce moral emotions [63] and foster empathy, as well as provide safe space to discuss concerns without criticism or repercussions.
Strengths and Limitations
We recognize the limitations of our study. Although our institution is a large regional tertiary referral center, limitation to a single center potentially reduces generalizability to other providers participating in pediatric end-of-life care. In qualitative research, however, validity is determined more through transferability of perceptions and experiences to other settings than generalizability to a population. [64] The ethical stress described by our respondents is similar in frequency to what has been reported in previous survey and qualitative studies; despite being obtained in a single center, our results are likely applicable to other pediatric centers that provide end-of-life care, and may be useful in informing educational efforts in those institutions. We acknowledge the possibility of selection bias, attributable to low overall survey response rate, or the minority of participants providing free-text comments. However, our total response rate for the survey was similar to what has been previously reported, [65,66] and the majority of pediatric deaths in this time period were captured with at least one completed survey and free text response. Though free-text responses lack the depth that full qualitative interviews provide, they have utility in identifying important issues not directly queried by close-ended survey questions, as well as informing future research. [64,66] The open-ended format of the free-response question gave respondents the opportunity to discuss a subject of their choosing, rather than prescribed topics serving the investigators’ aims, and allowed points to be raised that would otherwise not have been addressed. The free-text responses varied between respondents in length and quality; though only 51 respondents commented on ethical stress, the concerns they discussed were likely applicable to others. Respondents who have difficulty expressing themselves in writing, have limited time to complete the survey, or do not have a more neutral or positive experience are less likely to comment. [66] This may have introduced bias, as respondents who are more articulate, have more time to respond or have a particularly strong opinion may be overrepresented. Another potential source of bias is that providers were able to complete a survey for each patient’s death in which they provided end-of-life care. De-identification of the survey responses limited our ability to identify whether the same provider completed the survey on multiple patients.
Future Directions / Implications for Practice
Based on these findings, additional exploration of the ethical challenges faced by pediatric providers during end-of-life care is needed. Further inquiry of all members of the interprofessional care team, as well as of patients’ families, will better inform educational efforts for providers and improve patient care in these medically, emotionally, and ethically complex cases. Further investigation of the frequency and nature of ethical concerns and ethical stress following pediatric death, as well as the consequences for providers of experiencing it, is warranted. Trial and evaluation of prospective, interprofessional ethics education and support in high mortality pediatric inpatient units may also be valuable in identifying ways to mitigate ethical stress for providers of pediatric end-of-life care.
We would like to thank Dr. James Azim and Melanie Halsey for creation and distribution of the survey and Dr. Kenneth Pituch for his assistance in this project.
The authors have disclosed no conflicts of interest.

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Affiliations
Stephanie Kukora
Division of Neonatal-Perinatal Medicine
Department of Pediatrics, University of Michigan Ann Arbor, MI
Center for Bioethics and Social Sciences in Medicine
University of Michigan, Ann Arbor, MI
Naomi Laventhal
Division of Neonatal-Perinatal Medicine
Department of Pediatrics, University of Michigan Ann Arbor, MI
Center for Bioethics and Social Sciences in Medicine
University of Michigan, Ann Arbor, MI
Janice Firn
Center for Bioethics and Social Sciences in Medicine
University of Michigan, Ann Arbor, MI
Patricia Keefer
Department of Pediatrics
University of Michigan , Ann Arbor, MI
Correspondence
Stephanie Kukora
Division of Neonatal-Perinatal Medicine
Department of Pediatrics
Mott Children’s Hospital
University of Michigan Medical Center
8-621 C&W Mott Hospital
1540 E. Hospital Drive, SPC 4254
Ann Arbor, MI 48109-4254
skukora@med.umich.edu
734-763-4109
Endnotes
1. Garros D. Moral Distress in the Everyday Life of an Intensivist. Front Pediatr. 2016;4:91. doi:10.3389/fped.2016.00091
2. Robins PM, Meltzer L, Zelikovsky N. The experience of secondary traumatic stress upon care providers working within a children’s hospital. J Pediatr Nurs. 2009;24(4):270-279. doi:10.1016/j.pedn.2008.03.007
3. Prentice T, Janvier A, Gillam L, Davis PG. Moral distress within neonatal and paediatric intensive care units: a systematic review. Arch Dis Child. 2016;101(8):701-708. doi:10.1136/archdischild-2015-309410
4. Sundin-Huard D, Fahy K. Moral distress, advocacy and burnout: theorizing the relationships. Int J Nurs Pract. 1999;5(1):8-13.
5. Weintraub AS, Geithner EM, Stroustrup A, Waldman ED. Compassion fatigue, burnout and compassion satisfaction in neonatologists in the US. J Perinatol. August 2016. doi:10.1038/jp.2016.121
6. Meadors P, Lamson A. Compassion fatigue and secondary traumatization: provider self care on intensive care units for children. J Pediatr Health Care Off Publ Natl Assoc Pediatr Nurse Assoc Pract. 2008;22(1):24-34. doi:10.1016/j.pedhc.2007.01.006
7. Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet Lond Engl. 2009;374(9702):1714-1721. doi:10.1016/S0140-6736(09)61424-0
8. American Academy of Pediatrics. Committee on Bioethics. Institutional ethics committees. Committee on Bioethics. Pediatrics. 2001;107(1):205-209.
9. McDougall RJ, Notini L. What kinds of cases do paediatricians refer to clinical ethics? Insights from 184 case referrals at an Australian paediatric hospital. J Med Ethics. 2016;42(9):586-591. doi:10.1136/medethics-2015-103025
10. Johnson L-M, Church CL, Metzger M, Baker JN. Ethics consultation in pediatrics: long-term experience from a pediatric oncology center. Am J Bioeth AJOB. 2015;15(5):3-17. doi:10.1080/15265161.2015.1021965
11. Thomas SM, Ford PJ, Weise KL, Worley S, Kodish E. Not just little adults: a review of 102 paediatric ethics consultations. Acta Paediatr. 2015;104(5):529-534. doi:10.1111/apa.12940
12. Morrison W, Womer J, Nathanson P, et al. Pediatricians’ Experience with Clinical Ethics Consultation: A National Survey. J Pediatr. 2015;167(4):919-924.e1. doi:10.1016/j.jpeds.2015.06.047
13. DuVal G, Sartorius L, Clarridge B, Gensler G, Danis M. What triggers requests for ethics consultations? J Med Ethics. 2001;27 Suppl 1:i24-29.
14. Pavlish CL, Hellyer JH, Brown-Saltzman K, Miers AG, Squire K. Barriers to Innovation: Nursesʼ Risk Appraisal in Using a New Ethics Screening and Early Intervention Tool. Adv Nurs Sci. 2013;36(4):304-319. doi:10.1097/ANS.0000000000000004
15. Bridges CM. Letter to the Editor: Adv Nurs Sci. 2014;37(3):193-194. doi:10.1097/ANS.0000000000000032
16. Zuzelo PR. Exploring the moral distress of registered nurses. Nurs Ethics. 2007;14(3):344-359. doi:10.1177/0969733007075870
17. Corley MC. Nurse moral distress: a proposed theory and research agenda. Nurs Ethics. 2002;9(6):636-650. doi:10.1191/0969733002ne557oa
18. Berger JT. Moral Distress in Medical Education and Training. J Gen Intern Med. 2014;29(2):395-398. doi:10.1007/s11606-013-2665-0
19. Giubilini A, Milnes S, Savulescu J. The Medical Ethics Curriculum in Medical Schools: Present and Future. J Clin Ethics. 2016;27(2):129-145.
20. Eckles RE, Meslin EM, Gaffney M, Helft PR. Medical ethics education: where are we? Where should we be going? A review. Acad Med J Assoc Am Med Coll. 2005;80(12):1143-1152.
21. Campbell AV, Chin J, Voo T-C. How can we know that ethics education produces ethical doctors? Med Teach. 2007;29(5):431-436. doi:10.1080/01421590701504077
22. Yarborough M, Jones T, Cyr TA, Phillips S, Stelzner D. Interprofessional education in ethics at an academic health sciences center. Acad Med J Assoc Am Med Coll. 2000;75(8):793-800.
23. Lennon-Dearing R, Lowry LW, Ross CW, Dyer AR. An interprofessional course in bioethics: Training for real-world dilemmas. J Interprof Care. 2009;23(6):574-585. doi:10.3109/13561820902921621
24. Aveyard H, Edwards S, West S. Core topics of health care ethics. The identification of core topics for interprofessional education. J Interprof Care. 2005;19(1):63-69. doi:10.1080/13561820400021692
25. Alfandre D, Rhodes R. Improving ethics education during residency training. Med Teach. 2009;31(6):513-517. doi:10.1080/01421590802206739
26. Stirrat GM, Johnston C, Gillon R, Boyd K, on behalf of the Medical Education Working Group of the Institute of Medical Ethics and associated signatories. Medical ethics and law for doctors of tomorrow: the 1998 Consensus Statement updated. J Med Ethics. 2010;36(1):55-60. doi:10.1136/jme.2009.034660
27. Browne A, Carpenter C, Cooledge C, et al. Bridging the professions: an integrated and interdisciplinary approach to teaching health care ethics. Acad Med J Assoc Am Med Coll. 1995;70(11):1002-1005.
28. Landry JT, Valiani S, Foreman TC, Patel RV. Development of an ethics education curriculum for critical care trainees in Canada: from knowledge synthesis to bedside application. Int J Ethics Educ. 2016;1(1):57-68. doi:10.1007/s40889-015-0006-3
29. Svantesson M, Lofmark R, Thorsen H, Kallenberg K, Ahlstrom G. Learning a way through ethical problems: Swedish nurses’ and doctors’ experiences from one model of ethics rounds. J Med Ethics. 2008;34(5):399-406. doi:10.1136/jme.2006.019810
30. Cavaliere TA, Daly B, Dowling D, Montgomery K. Moral distress in neonatal intensive care unit RNs. Adv Neonatal Care Off J Natl Assoc Neonatal Nurses. 2010;10(3):145-156. doi:10.1097/ANC.0b013e3181dd6c48
31. Trotochaud K, Coleman JR, Krawiecki N, McCracken C. Moral distress in pediatric healthcare providers. J Pediatr Nurs. 2015;30(6):908-914. doi:10.1016/j.pedn.2015.03.001
32. Sauerland J, Marotta K, Peinemann MA, Berndt A, Robichaux C. Assessing and addressing moral distress and ethical climate Part II: neonatal and pediatric perspectives. Dimens Crit Care Nurs DCCN. 2015;34(1):33-46. doi:10.1097/DCC.0000000000000083
33. Sannino P, Giannì ML, Re LG, Lusignani M. Moral distress in the neonatal intensive care unit: an Italian study. J Perinatol Off J Calif Perinat Assoc. 2015;35(3):214-217. doi:10.1038/jp.2014.182
34. Solomon MZ. New and Lingering Controversies in Pediatric End-of-Life Care. PEDIATRICS. 2005;116(4):872-883. doi:10.1542/peds.2004-0905
35. Janvier A, Nadeau S, Deschênes M, Couture E, Barrington KJ. Moral distress in the neonatal intensive care unit: caregiver’s experience. J Perinatol Off J Calif Perinat Assoc. 2007;27(4):203-208. doi:10.1038/sj.jp.7211658
36. Wall S, Austin WJ, Garros D. Organizational Influences on Health Professionals’ Experiences of Moral Distress in PICUs. HEC Forum. 2016;28(1):53-67. doi:10.1007/s10730-015-9266-8
37. Catlin A, Armigo C, Volat D, et al. Conscientious objection: a potential neonatal nursing response to care orders that cause suffering at the end of life? Study of a concept. Neonatal Netw NN. 2008;27(2):101-108. doi:10.1891/0730-0832.27.2.101
38. Hefferman P, Heilig S. Giving “moral distress” a voice: ethical concerns among neonatal intensivecare unit personnel. Camb Q Healthc Ethics CQ Int J Healthc Ethics Comm. 1999;8(2):173-178.
39. McGibbon E, Peter E, Gallop R. An institutional ethnography of nurses’ stress. Qual Health Res. 2010;20(10):1353-1378.doi:10.1177/1049732310375435
40. Lee KJ, Dupree CY. Staff experiences with end-of-life care in the pediatric intensive care unit. J Palliat Med. 2008;11(7):986-990. doi:10.1089/jpm.2007.0283
41. Yam BM, Rossiter JC, Cheung KY. Caring for dying infants:experiences of neonatal intensive care nurses in Hong Kong. J Clin Nurs. 2001;10(5):651-659.
42. Davies B, Clarke D, ConnaughtyS, et al. Caring for dying children: nurses’ experiences. Pediatr Nurs. 1996;22(6):500-507.
43. Molloy J, Evans M, Coughlin K.Moral distress in the resuscitation of extremely premature infants.Nurs Ethics. 2015;22(1):52-63. doi:10.1177/0969733014523169
44. Qualtrics, Provo, Utah, USA. 2016, Available from:http://www.qualtrics.com
45. Dedoose Version 7.0.23, webapplication for managing, analyzing, and presenting qualitative and mixed method research data (2016). Los Angeles, CA: SocioCultural Research Consultants, LLC (www.dedoose.com).
46. Sinkovics RR, Alfoldi EA. Progressive focusing and trustworthiness in qualitative research: the enabling role of computer-assisted qualitative data analysis software (CAQDAS).Manag Int Rev. 2012;52(6):817-845.doi:10.1007/s11575-012-0140-5
47. Fielding NG, Lee RM.Computer analysis and qualitative research. London: SAGE; 1998.
48. Charmaz, K. “Grounded theory: objectivist and contructivist methods.” In: The Handbook of Qualitative Research. Edited by N.K. Denzin and Y. Lincoln. Thousand Oaks, CA: Sage Publications, Inc.; 2000.
49. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77-101.doi:10.1191/1478088706qp063oa
50. Hursthouse R, Pettigrove G. “Virtue Ethics.” The Stanford Encyclopedia of Philosophy (Winter 2016 Edition),Edward N. Zalta (ed.), URL = <https:// plato.stanford.edu/archives/ win2016/entries/ethics-virtue/>.
51. Kraut, Richard, “Aristotle’s Ethics.” The Stanford Encyclopedia of Philosophy (Summer 2017Edition), Edward N. Zalta (ed.), URL = <https://plato.stanford.edu/archives/ sum2017/entries/aristotle-ethics/>.
52. Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med 1982. 1997;44(5):681-692.
53. Moon JY, Kim J-O. Ethics in the Intensive Care Unit. Tuberc Respir Dis. 2015;78(3):175. doi:10.4046/trd.2015.78.3.175
54. Nester J. The Importance of inter-professional practice and education in the era of accountable care. N C Med J. 2016;77(2):128- 132. doi:10.18043/ncm.77.2.128
55. Joseph S, Diack L, Garton F,Haxton J. Interprofessional education in practice. Clin Teach. 2012;9(1):27-31.doi:10.1111/j.1743-498X.2011.00486.x
56. Health Professions Education: A Bridge to Quality. Washington, D.C.: National Academies Press; 2003. doi:10.17226/10681
57. Goold SD, Stern DT. Ethics and professionalism: what does a resident need to learn? Am J Bioeth. 2006;6(4):9-17.doi:10.1080/15265160600755409
58. Kon AA. Resident-generated versus instructor-generated cases in ethics and professionalism training. Philos Ethics Humanit Med PEHM. 2006;1(1): E10. doi:10.1186/1747-5341-1-10
59. Klingensmith ME. Teaching ethics in surgical training programs using a case-based format. J Surg Educ. 2008;65(2):126-128.doi:10.1016/j.jsurg.2007.12.001
60. Pavlish C, Brown-Saltzman K, Fine A, Jakel P. Making the call: aproactive ethics framework. HEC Forum Interdiscip J Hosp Ethical Leg Issues. 2013;25(3):269-283.doi:10.1007/s10730-013-9213-5
61. Splaine ME, Nelson WA,Gardent PB. Editorial: Broadening implementation of a preventiveethics approach. Jt Comm J Qual Patient Saf. 2012;38(3):99-102.
62. Charon R. Narrative medicine: a model for empathy, reflection, profession, and trust. JAMA. 2001;286(15):1897. doi:10.1001/jama.286.15.1897
63. Fiester A. Contentious conversations: using mediation techniques in difficult clinical ethics consultations. J Clin Ethics. 2015;26(4):324-330.
64. O’Cathain A, Thomas KJ. “Any other comments?” Open questions on questionnaires – a bane or a bonus to research? BMC Med Res Methodol. 2004;4(1). doi:10.1186/1471-2288-4-25
65. Burns KEA, Duffett M, Kho ME, et al. A guide for the design and conduct of self-administered surveys of clinicians. Can Med Assoc J. 2008;179(3):245-252. doi:10.1503/cmaj.080372
66. Garcia J, Evans J, Reshaw M. “Is there anything else you would like to tell us’’ – Methodological issues in the use of free-text comments from postal surveys. Qual Quant. 2004;38(2):113-125. doi:10.1023/ B:QUQU.0000019394.78970.df
67. Rokeach M. The Nature of Human Values. New York: The Free Press; 1973.
68. Tucker Edmonds B, Torke AM, Helft P, Wocial LD. Doctor, what would you do? An answer for patients requesting advice about value-laden decisions. Pediatrics. 2015;136(4):740-745.doi:10.1542/peds.2015-1808
69. Folkman S, Lazarus RS. An analysis of coping in a middle-aged community sample. J Health Soc Behav. 1980;21(3):219.doi:10.2307/2136617
70. Barr H, ed. Effective Interprofessional Education: Argument, Assumption, and Evidence. Oxford; Malden, Mass: Blackwell Pub; 2005.