There is no excerpt because this is a protected post.
There is no excerpt because this is a protected post.

Offering sanctuary to those fleeing war is a pressing human rights issues in the world today. Globally, there are currently 25.4 million people forced to leave their home to seek safety. Half of these people are children. Despite these staggering statistics, governments seem to have ignored their duty of care to children.

Legal and social precedent support broad parental discretion in the absence of immediate and severe endangerment of the minor’s welfare. However, in many cases of maltreatment, suspected or substantiated, parents retain PDM rights. The possibility of a guardian who is both surrogate and cause of harm threatens the conventional decision-making model; this paper offers an analysis of the primary challenges and shows that many of the ethical questions arise as the decision-making process unfolds and information is gathered.

This article highlights the importance of psychological and medical evaluations for asylum seekers in the United States, and identifies physicians and other healthcare professionals as uniquely situated for this work. This paper outlines the benefits and drawbacks to such evaluations and addresses their utility in immigration law, ultimately calling for increased clinician involvement in pro bono evaluations.
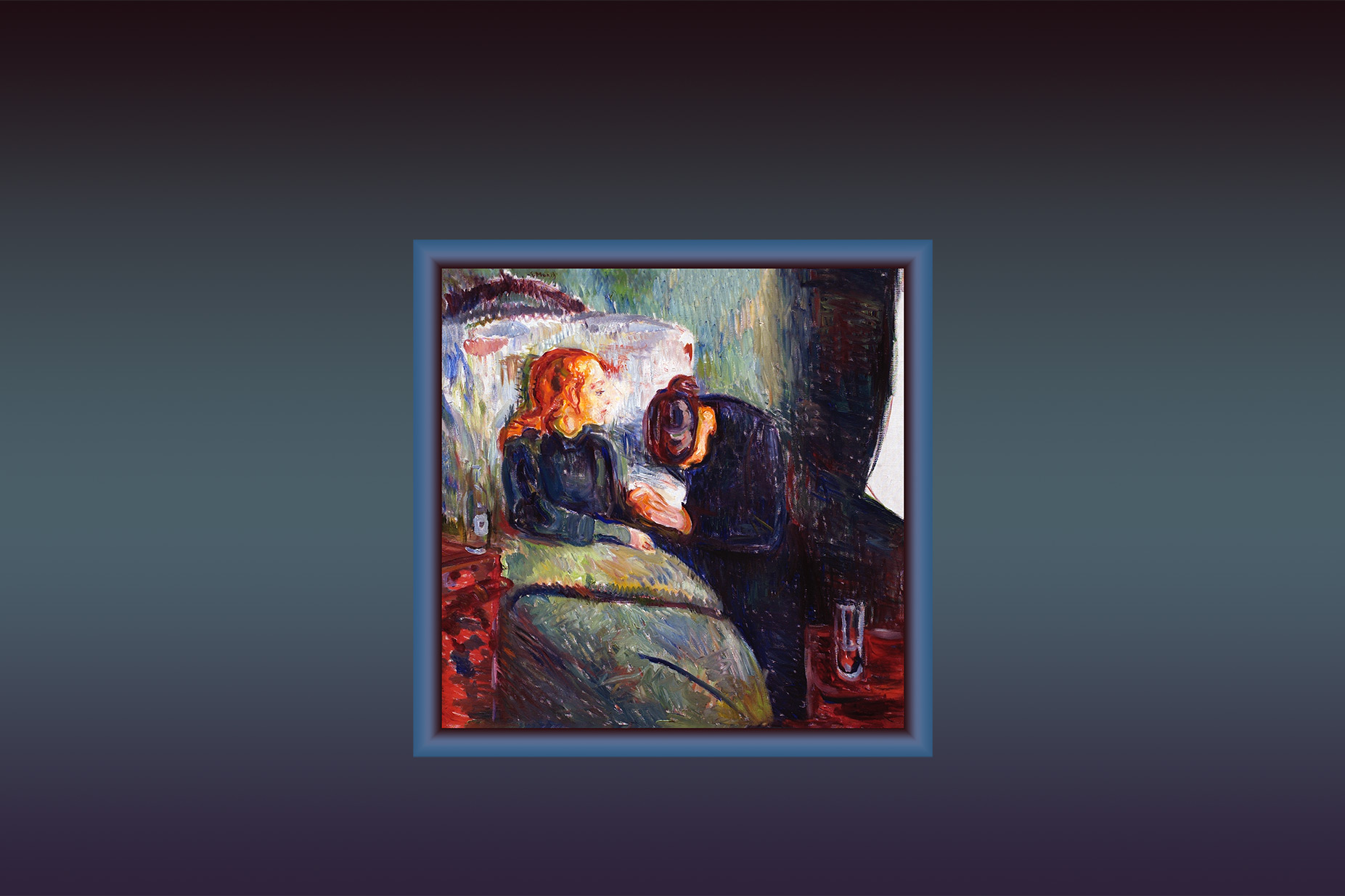
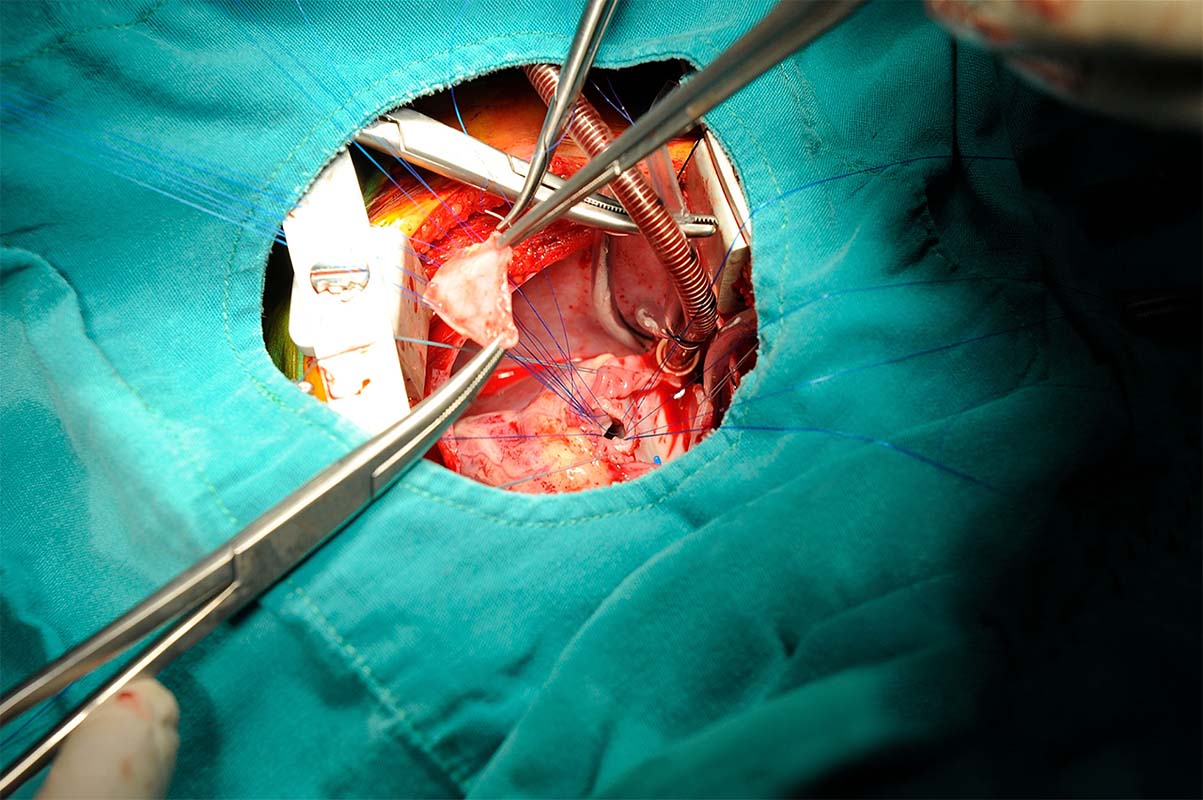
Editorial volume 21 number 2: We have introduced a number of new elements to the Pediatric Ethicscope website over the past several weeks. These changes were prompted by several requests from readers, and most of the changes are aimed at aiding readers wanting to cite and download Pediatric Ethicscope articles for research or teaching purposes. About the cover; about the articles.

In recent years, the unique role of medical professionals in the asylum adjudication process has been thrown into sharp relief as asylum applications surge, with over one million pending cases backlogged in the U.S. asylum system as of August 2019. Medical evaluations dramatically increase the likelihood of an individual obtaining asylum. The author examines the role medical trainees play in this process.
How did we get here? Mara, now nearly 17-years-old, was born with a neurogenic bladder. Up until two years ago, she was a model patient. No one worried about her adherence with self-catheterization or medications. She was optimistic about her future, cared about her health, and we looked forward to her bright and open future. But now Mara says,
“I don’t care.”